This article is published with the kind permission of “Defence and Security Alert (DSA) Magazine” New Delhi-India
One of the greatest disaster scenarios is the use of WMDs by non-state actors. India is enhancing its commitment to nuclear energy. These reactors are also potential targets for mass casualty terror strikes. The recent Tsunami in Japan led to a nuclear meltdown on an unprecedented scale. CBRN (Chemical, Biological, Radioactive and Nuclear Weapons) terrorism or catastrophes with a radiological dimension triggered by natural or man-made disasters are an eventuality that we must be well prepared for in this country. The recent Delhi High Court blast also highlighted the need for casualty management in such scenarios. A very timely and well written article by a Greek Brigadier General on CBRN response by hospitals in the event of WMD based terror strike or natural disaster. This article focuses on hospital CBRN preparedness in megapolis environment and comments on the attitude of state high officials involved in CBRN planning.
 |
Megapolis
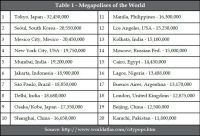
A megapolis (combined Greek word: mega [or megalo] = huge and polis = city), also known as megalopolis or megaregion, is a clustered network of cities with a population of about 10 million or more and at least 2,000 persons / km2 (i.e. Delhi has a land of 1,483 km² and a population density of 9,296 people / km2). Modern interlinked ground transportation corridors, such as rail and highway, often aid in the development of megalopolises. In the top-20 of most populated cities worldwide (Table 1), there are three Indian megalopolises — Mumbai, Delhi and Kolkata.
 |
| Click to enlarge |
Hospitals as targets
Since the beginning of the 21st century, hospitals both in peace and war were considered as sacred areas respected by adversaries either in urban environment or in the operational field. Starting with Cama Hospital in the Mumbai 2008 multiple terrorist attacks many instances of hospitals’ attacks have been recorded in various countries around the globe (i.e. Military Hospital in Kabul, Afghanistan [2011], Misrata Hospital in Libya [2011], etc.). Therefore it is obvious that hospitals represent an attractive soft target for modern terrorists. If by attacking hospitals you kill the hope for the people involved in a terrorist incident then it is like killing them twice.
CBRNE incident site
In case of a real CBRN terrorist incident in a megapolis environment there are two things that you must have always in mind. The first one is that planning should follow major anthropocentric patterns. This means that every plan should always answer the following question: “What would be my personal reaction if involved in such an incident?”
The second one refers to certain statistics that are crucial to remember and have to do with the crowd behaviour. In that respect it is estimated that after the CBRN incident approximately 20 per cent of those involved will remain in place (dead, severely wounded and / or contaminated). The remaining 80 per cent will flee to all possible directions seeking medical assistance or if not wounded or contaminated will go home. The third important statistic is that the ratio of truly contaminated vs “worried well” is 1:5. This will soon overwhelm hospitals and collapse even the most organised and advanced medical systems worldwide. The experience from Tokyo sarin release shows that 84.5 per cent of those involved went to 169 hospitals and clinics all over the capital by their own means. The above numbers stress the need to invest on hospitals’ CBRN defence instead of classic “golden hour” first responders. The latter will certainly go there but they will arrive late (due to very heavy traffic and big dimensions of decontamination vehicles) and most probably those who are severely contaminated / wounded would be dead. So why invest all that money on first responders that will go there late instead of investing on health infrastructure that will surely accept those escaped and have a good chance to survive? No need to say that medical consequences of CBRN agents’ release might last for decades — as is the case with Iran-Iraq chemical war casualties.
The experience from Tokyo sarin release shows that 84.5 per cent of those involved went to 169 hospitals and clinics all over the capital by their own means. The above numbers stress the need to invest on hospitals’ CBRN defence instead of classic “golden hour” first responders. The latter will certainly go there but they will arrive late (due to very heavy traffic and big dimensions of decontamination vehicles) and most probably those who are severely contaminated / wounded would be dead
Hospital CBRN defence
A hospital might be very close or adjacent to the incident site or far to very far away. If very close then reaction time is minimal if none. This means that the EMS section of the hospital must be able to go to “red alert” within minutes. This takes a lot of training, specialised equipment, modern planning and open minded individuals that understand the nature of the event. Hospitals that are in more distant areas might have enough time to prepare although in many instances nobody will go there no matter how prepared they are. It is obvious that all hospitals and clinics both public and private should be equally prepared to accept mass CBRN casualties in case of a terrorist event. One might say that casualties should be “guided” to certain specialised hospitals and close all those that do not have the facilities to deal with CBRN contaminated victims. Now ask yourself what would be your reaction if arriving in such a hospital with your contaminated / wounded child and someone was informing you that it is closed and you have to go to another far away hospital …
Hospital preparedness
The good thing with hospital CBRN preparedness is that most of the equipment needed is already available within the hospital. Of course there is certain additional equipment that is specifically made for contaminated environments (i.e. field respirator with NBC filter) but apart from these the remaining are every day’s materials and resources.
The important parameter in hospital defence is to keep contamination away from the hospital, working medical personnel and existing patients. In that respect the CBRN Response Unit of the hospital should be deployed outside the hospital; preferably at the parking lot of the hospital. The response unit is composed by several stations that facilitate the arriving casualties. To start with it is very important to have a fence around the hospital. If there is no fence then the control of the arriving citizens would be difficult if not impossible to control. But even with a fence someone might try to override it if not willing to stay in line. This means that security personnel should be deployed as well guarding the inner territory of the hospital. The usual security personnel of the hospital it is for sure will not be able to contribute since they do not possess the abilities, training and personal protective equipment to fulfill their mission in a contaminated environment. Police support is the only solution available.
 |
| Click to enlarge |
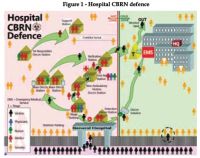
In case of a real event (Figure 1):
1) All casualties / victims presenting to the hospital will enter hospital from one and only gate.
2) All casualties / victims will go through “Detection Station” where if negative they will proceed and walk through a decontamination solution on their way to the EMS department of the hospital. If positive they will proceed to “Triage Station”.
3) Casualties will be either able to walk or on stretchers. In the first case they proceed to “Mass Decontamination Stations” for thorough decontamination.
4) If non-ambulatory they will be transported to the “Non-Ambulatory Victims Decontamination Station”. When decontamination is over they will be rolled to adjusting “First Aid Station” for provision of life saving first aids (antidotes, respiratory support, bleeding control). Antidotes can be given at the “Triage Station” as well depending on the situation.
5) When victims from both the “Mass Decontamination Station” and “First Aid Station” are ready and “clean” they proceed through the “Verification Station” that confirms the success of decontamination. If negative they end up in the main triage area of the hospital at the “cold zone”. If positive they have to repeat decontamination process.
6) At the “Triage Station” hospital personnel will decide who needs immediate hospitalisation and who can go home with written instructions in case a relapse evolves within the next few hours. One of the main tasks of the triage personnel is to get rid of “worried well” that represent a functional threat to the continuity of the hospital work due to their vast numbers.
7) First responders either from the hospital or from other state departments and organisations need to have their own decontamination line. This is mandatory and this line should be deployed before starting to accept contaminated casualties. “Save the saver to operate” is the main reason but also the rule in all CBRN operations.

 von
von